Partial (Unicompartmental) Knee Replacement
Indications for Partial Knee Replacement
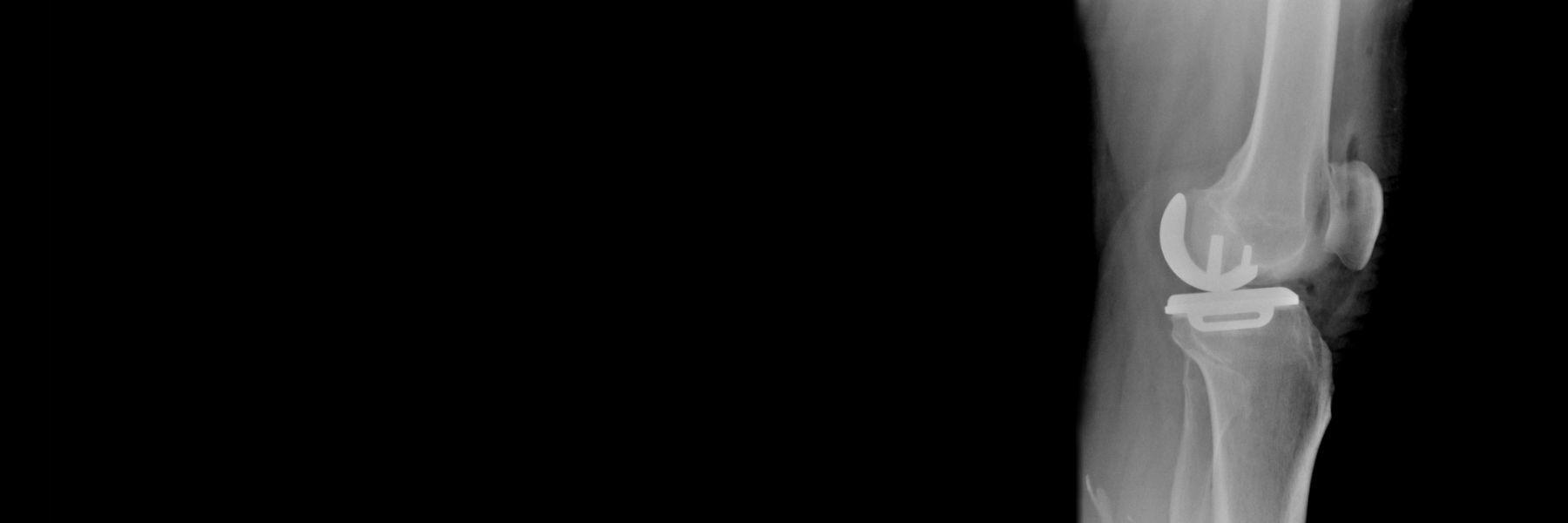
Not all patients presenting with an arthritic knee will have wear and tear in all three compartments (medial, lateral, and patellofemoral) of the knee. For patients whose cartilage is only worn down in a single, specific knee compartment, a partial (unicompartmental) knee replacement may be an option.
Of course, not everyone is necessarily a good candidate for a partial knee replacement. A thorough workup, including history and physical exam, a panel of x-rays, and occasionally advanced imaging such as MRI, may be required to fully elucidate the source of the patient’s knee problem and determine the most appropriate course of action for that patient. Surgery is never a “one size fits all” endeavor, and every attempt is made to customize the treatment plan to the individual patient in order to achieve the best possible outcome.
Historical Perspective
Partial knee replacement has been an option for several decades. Recent improvements in the implant materials, surgical technique, and instrumentation have enhanced the long-term performance of these devices. The main advantage of a unicompartmental knee replacement is that the surgery is limited solely to the region of the knee (either medial, lateral, or patellofemoral compartment) where there is arthritic damage; the other two intact compartments are left untouched. Additionally, the cruciate ligaments and the meniscus in the normal compartment are all left intact. This can result in a knee that has a feel and functionality that seems “more normal” for the patient and may facilitate enhanced participation in sports and other activities.
Surgical Technique
Similar to a total knee replacement, a partial knee replacement requires careful balancing of the flexion and extension spaces in order to achieve a well functioning reconstruction. This may involve releases of ligaments that are too tight, resection of bone spurs which can alter the knee balance, and avoiding overcorrection of the joint deformity. A well gap-balanced surgery ensures that the patient’s knee feels equally stable in both flexion and extension. Using robotic-assistance and computer navigation helps to increase the accuracy and precision of component placement.
Post-Operative Recovery
After a partial knee replacement, patients may immediately weight bear as tolerated, with no restrictions. The range of motion of the knee is progressively improved over the first few weeks. Specific physical therapy protocols are available on the website and will be initiated by your physical therapist.
For the first 2-4 weeks, patients are encouraged to walk, practice going up and down stairs, and generally resume the activities of daily living.
By 2-4 weeks, most patients have discontinued the need for a cane and are walking unsupported.
From 6-12 weeks, the patient will notice larger gains in physical therapy in terms of endurance, range of motion, and strength.
By 12 weeks, most patients are resuming sports and other activities, but may continue to see additional improvement even up through one year after surgery.
Frequently Asked Questions
The most important part of the implant is the bearing surface. This is the smooth, polished part of the implant that articulates at the level of the joint, allowing the low-friction motion which is required to walk normally. Over time, surgeons have tried many different combinations of bearing surfaces, each of which has certain advantages and drawbacks. The most predictable results are found using bearing surfaces that have stood the test of time, and have demonstrated decades-long survivorship in longitudinal registry studies.
The knee replacement prosthetic is a hinge-type articulation, consisting of the rounded condyles of the lower part of the thigh bone (the femur), flexing and extending along the flat surface of the upper part of the shin bone (the tibia). The femoral component, which re-surfaces the arthritic femoral condyles (similar to capping a tooth) is made of a very durable, polished metal, a cobalt-chrome alloy. This implant is cemented into the femur using high-viscosity bone cement.
On the tibial side, the bearing surface is made of a highly cross-linked polyethylene liner and is locked into the tibial baseplate, which is made of titanium alloy. The tibial baseplate is cemented into the tibia using the same high-viscosity bone cement. Thus, the final bearing surface is metal-on-polyethylene.
Meet Dr. Gladnick:

Brian P. Gladnick, MD
Dr. Gladnick is a Magna Cum Laude graduate of the University of Delaware, where he was elected to Phi Beta Kappa. He went on to earn his medical degree from Cornell University in New York, where he received the T. Campbell Thompson Prize for excellence in Orthopaedic Surgery. He completed his residency in Orthopaedic Surgery at the Hospital for Special Surgery/Cornell Medical Center in New York, followed by a fellowship in Adult Total Joint Reconstruction at the OrthoCarolina Hip and Knee Center in Charlotte. He now serves as the fellowship ...




