Total Knee Replacement
Indications for Total Knee Replacement
There are a variety of conditions which may result in a worn-out knee joint. Most common is osteoarthritis, a “wear-and-tear” condition in which the protective cartilage covering of the joint gradually thins out over time, resulting in progressive knee pain and stiffness.
More rarely seen are the inflammatory types of arthritis, such as rheumatoid arthritis, which is a medical condition resulting in progressive cartilage loss.
Previous injury or deformity to the knee or limb results in changes to the local biomechanical properties of the knee joint, which may accelerate cartilage loss.
When the joint damage has become sufficiently severe, and the patient’s quality of life is beginning to suffer, a total knee replacement may be indicated.
Historical Perspective
Total knee replacement surgery is a highly successful procedure for eliminating the pain and stiffness associated with knee arthritis. Most simply put, this procedure involves removing the damaged cartilage and bone from the inside of the knee and then replacing the weight-bearing surfaces with a new implant (similar to capping a tooth) that allows a smooth arc of motion and the ability to walk without pain.
Over time, the surgery techniques, implants, and instrumentation have continued to evolve in order to improve patient outcomes. Ensuring that a patient undergoing this surgery will have a good result requires careful attention to the patient’s limb alignment and meticulous handling of the soft tissues.
Surgical Technique
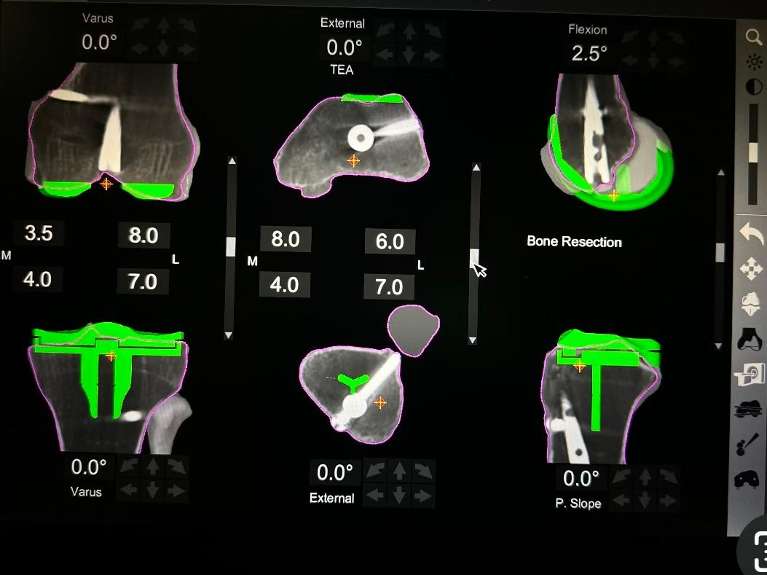
During a knee replacement, the surgeon designs the space between the tibia and femur to be an equal, rectangular “gap” in both flexion and extension, prior to finishing bone preparation and inserting the implants. This involves releases of ligaments that are too tight, resection of bone spurs which can alter the knee balance, and adjusting the rotational alignment of the femoral component so that it parallels the plane of the tibial component. Using robotic arm assistance or computer navigation increases the accuracy and precision of component implantation.
A well gap-balanced surgery ensures that the patient’s knee feels equally stable in both flexion and extension, and the patella tracks normally throughout the arc of motion.
Post-Operative Recovery
After a total knee replacement, patients may immediately weight bear as tolerated, with no restrictions. The range of motion of the knee is progressively improved over the first few weeks. Specific physical therapy protocols are available on the website and will be initiated by your physical therapist.
For the first 2-4 weeks, patients are encouraged to walk, practice going up and down stairs, and generally resume the activities of daily living.
By 2-4 weeks, most patients have discontinued the need for a cane and are walking unsupported.
From 6-12 weeks, the patient will notice larger gains in physical therapy in terms of endurance, the range of motion, and strength.
Usually, by 12 weeks, the patient is starting to feel close to normal and is resuming most activities, but many patients continue to see ongoing improvement even up through one year after surgery.
Theresa R. ⭐⭐⭐⭐⭐
"Dr. Gladnick is AMAZING! I had to have my left knee replaced in 2016 and my right replaced in 2017. He has given me back my life!! I will now be able to do activities that I have not been able to participate in and now I can! I cannot explain how much Dr. Gladnick means to me. He is professional, extremely personable, and the best knee surgeon EVER! I HIGHLY recommend Dr. Gladnick - he is incredible."
Frequently Asked Questions
The most important part of the implant is the bearing surface. This is the smooth, polished part of the implant that articulates at the level of the joint, allowing the low-friction motion which is required to walk normally. Over time, surgeons have tried many different combinations of bearing surfaces, each of which has certain advantages and drawbacks. The most predictable results are found using bearing surfaces that have stood the test of time, and have demonstrated decades-long survivorship in longitudinal registry studies.
The knee replacement prosthetic is a hinge-type articulation, consisting of the rounded condyles of the lower part of the thigh bone (the femur), flexing and extending along the flat surface of the upper part of the shin bone (the tibia). The femoral component, which re-surfaces the arthritic femoral condyles (similar to capping a tooth) is made of a very durable, polished metal, a cobalt-chrome alloy. This implant is cemented into the femur using high-viscosity bone cement.
On the tibial side, the bearing surface is made of a highly cross-linked polyethylene liner and is locked into the tibial baseplate, which is made of titanium alloy. The tibial baseplate is cemented into the tibia using the same high-viscosity bone cement. Thus, the final bearing surface is metal-on-polyethylene.
Navigation involves the use of computer software to enhance implant positioning. Historically, surgeons have used a variety of handheld jigs to estimate the bone cuts made during surgery. The introduction of computer navigation has significantly improved the accuracy and precision of these bone cuts. Essentially, the computer software is used to calculate the center of the hip, knee, and ankle during surgery.
Once these points are registered, the mechanical axes of the femur and tibia are determined by the software, and the bone cuts are planned using these data. Multiple studies have now demonstrated that computer navigation improves both implant position and patient-reported outcomes in total knee replacement.
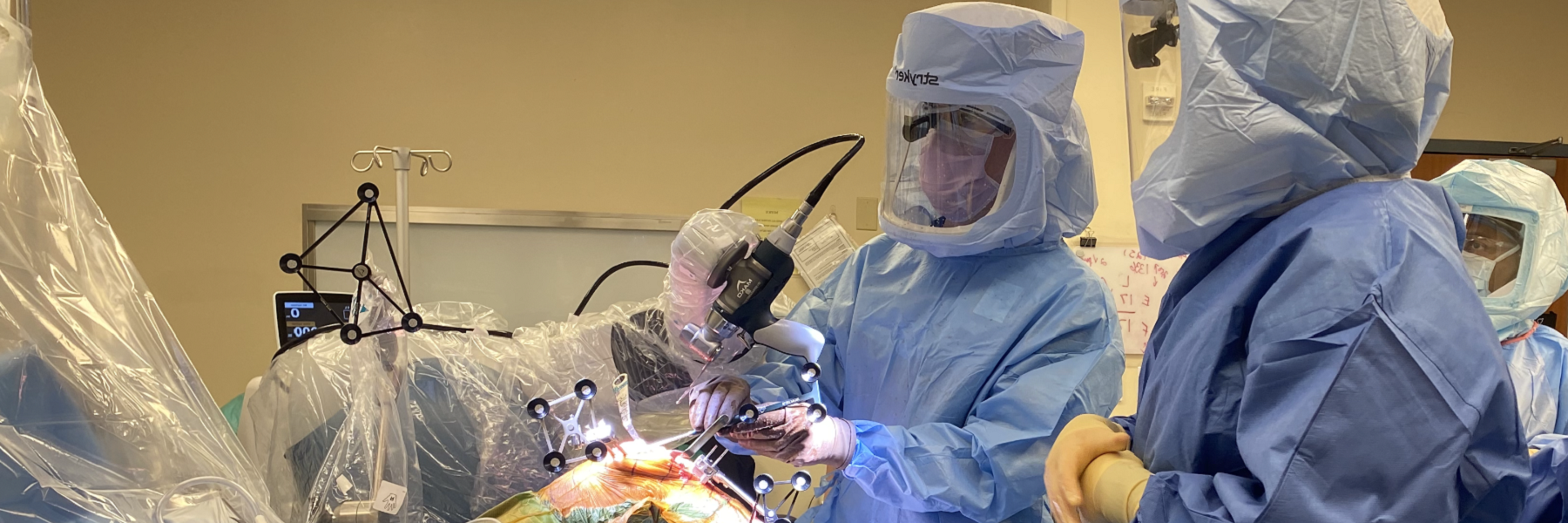
Robotic-assisted knee replacement expands upon the previous forms of computer navigation by using a haptic robotic arm, which is brought onto the surgical field to assist with the bone resections. The surgeon registers multiple anatomic checkpoints into the computer, creating a 3-dimensional map of the patient's knee which is matched to a preoperative CT scan. A virtual surgery is trialed on the computer, creating a plan which accurately reconstructs the mechanical axis of the limb while ensuring proper gap balancing. The robotic arm is then brought onto the sterile field and executes the surgical plan.
Meet Dr. Gladnick:

Brian P. Gladnick, MD
Dr. Gladnick is a Magna Cum Laude graduate of the University of Delaware, where he was elected to Phi Beta Kappa. He went on to earn his medical degree from Cornell University in New York, where he received the T. Campbell Thompson Prize for excellence in Orthopaedic Surgery. He completed his residency in Orthopaedic Surgery at the Hospital for Special Surgery/Cornell Medical Center in New York, followed by a fellowship in Adult Total Joint Reconstruction at the OrthoCarolina Hip and Knee Center in Charlotte. He now serves as the fellowship ...
Total Knee Replacement Technology
Robotic-Assisted and Computer-Navigated Knee Replacement
Historically, bone cuts during total and partial knee replacement have been made using manual alignment jigs. This requires the surgeon to use bony landmarks and their own experience to make the series of bony cuts required for implant insertion. While effective, performing these cuts manually does introduce a certain degree of variability into the procedure due to surgeon, patient, or implant-related factors. The use of robotics and computer navigation reduces this variability, and improves the surgeon's ability to place implants with a high degree of accuracy. Multiple points of reference using the patient's own anatomy are registered into the computer, and the implants can be modeled virtually onto a 3D reconstruction of the patient's bone. When the final plan is executed, the implant is then positioned to restore the patient's native anatomy and promote optimal soft tissue balance.




